SAN FRANCISCO, CA / ACCESS Newswire / January 30, 2025 / A new study published in JAMA Network Open has found that while procedural prescription denials curb immediate drug costs, some denials result in increased acute care utilization and costs, which outweigh any short-term savings.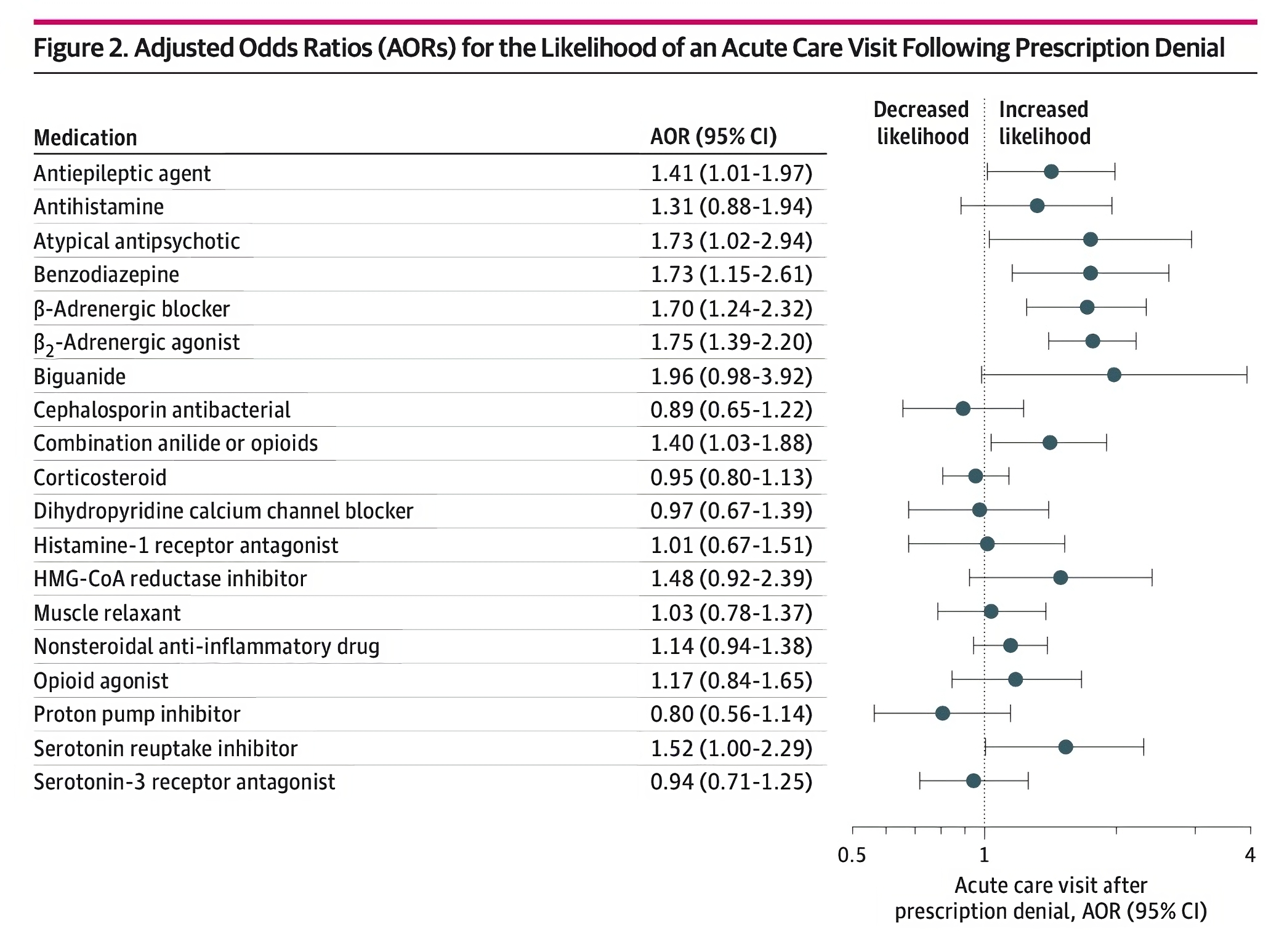
A procedural prescription denial occurs when a prescription is rejected due to administrative or procedural issues rather than medical necessity. Common reasons for procedural prescription denials include a patient requesting a refill too early, exceeding medication quantity allowed per prescription, being prescribed a medication not covered in the plan formulary, or being prescribed a medication that requires a prior authorization, among others.
In this large study of 19,725 Medicaid enrollees, researchers found that patients experiencing procedural prescription denials had a higher risk of physiologically related emergency department (ED) visits and hospitalizations compared with those without a denial in the subsequent 60 days. Denials in six medication classes were associated with net total medical spending increases ranging from $624 to $3,016 in additional expense per patient per year.
"This study implies that helping patients promptly resolve procedural denials can reduce both acute care utilizations and unnecessary healthcare costs," said Bhairavi Muralidharan, the lead author for the study and a data scientist at Waymark. "Ultimately, early interventions reinforce the goal of every Medicaid program - to provide accessible, cost-effective care to vulnerable populations."
Rising prescription costs in Medicaid have led many pharmacy benefit managers and health plans to implement procedural denials as a cost-containment measure. When patients are unable to obtain medications due to a prescription denial, they may be hospitalized or visit the ED due to an exacerbation of their chronic conditions. For example, a patient suffering from seizures may end up in the ED if their anti-seizure medication is denied. A previous study from Waymark published in the American Journal of Managed Care found that nearly 40% of ED visits and hospitalizations in Medicaid could be avoided through timely access to primary care, including medication support.
"There is a huge opportunity to reduce unnecessary acute care utilization and costs in Medicaid," said Jeffrey Tingen, co-author of the study and a Clinical Pharmacist Lead at Waymark. "This research shows that proper medication management, which includes addressing procedural prescription denials, can reduce avoidable ED visits and hospitalizations in the Medicaid population."
Researchers analyzed Medicaid data in two different states (n=19,725, Virginia and Washington). The study included patients with at least one pharmacy claim during the study period (January 1 to July 31, 2023) and focused on the 20 most commonly prescribed medication classes out of a total of 390. For each medication class, patients were assigned to either the exposure group (defined as having ≥ 1 procedural denial for a given medication class during the study period) or a control group (defined as having 0 denials for that class). The two groups were matched based on demographic features, clinical history and other aspects of medical care. Researchers evaluated acute care events (an ED visit or hospitalization) and associated costs within a 60-day period following the prescription denial, verifying whether the denial was medically related to the reason for the acute care event.
"While earlier studies have shown that procedural prescription denials are more common in Medicaid than other forms of insurance, empirical research on the effect of these denials on healthcare utilization and long-term costs is scarce," said Sadiq Y. Patel, VP of Data Science and AI at Waymark. "These findings can help Medicaid health plans inform their policy decisions, including formulary, coverage, prior authorization requirements, claim denials and approvals, and payments based on drug classes."
Waymark's multidisciplinary care team includes clinical pharmacists and pharmacy technicians who help patients access and manage their medications, including proactively contacting them to help resolve procedural denials. For example, Waymark's pharmacy team routinely fills out prior authorization forms and works with providers to mitigate the risk of a procedural denial. In collaboration with Waymark's community health workers, these teams complete "weekend tuck-ins" on Thursdays and Fridays to ensure patients have necessary medications, reducing the likelihood of an acute exacerbation over the weekend. A 2024 study published in NEJM Catalyst found that Waymark reduced all-cause hospital and ED visits by 22.5% for rising-risk patients in its first year of service.
The full article titled "Procedural Prescription Denials and Risk of Acute Care Utilization and Spending Among Medicaid Patients" was published in JAMA Network Open. The authors of this article are Bhairavi Muralidharan, MSE of Waymark; Sanjay Basu, PhD, MD of Waymark; Jeffrey Tingen, MBA, PharmD of Waymark; and Sadiq Y. Patel, PhD, MS, MSW of Waymark.
Contact Information
Iman Rahim
Communications
iman.rahim@waymarkcare.com
SOURCE: Waymark
View the original press release on ACCESS Newswire





